Abstract
Previous literature indicates that pre-diagnostic diabetes and blood glucose levels are inversely related to glioma risk. To replicate these findings and determine whether they could be attributed to excess glucose consumption by the preclinical tumour, we used data from the Apolipoprotein MOrtality RISk (AMORIS) (n = 528,580) and the Metabolic syndrome and Cancer project (Me-Can) cohorts (n = 269,365). We identified individuals who were followed for a maximum of 15 years after their first blood glucose test until glioma diagnosis, death, emigration or the end of follow-up. Hazard ratios (HRs), 95% confidence intervals (CIs) and their interactions with time were estimated using Cox time-dependent regression. As expected, pre-diagnostic blood glucose levels were inversely related to glioma risk (AMORIS, P trend = 0.002; Me-Can, P trend = 0.04) and pre-diagnostic diabetes (AMORIS, HR = 0.30, 95% CI 0.17 to 0.53). During the year before diagnosis, blood glucose was inversely associated with glioma in the AMORIS (HR = 0.78, 95% CI 0.66 to 0.93) but not the Me-Can cohort (HR = 0.99, 95% CI 0.63 to 1.56). This AMORIS result is consistent with our hypothesis that excess glucose consumption by the preclinical tumour accounts for the inverse association between blood glucose and glioma. We discuss additional hypothetical mechanisms that may explain our paradoxical findings.
Similar content being viewed by others
Introduction
Glioma is a heterogeneous primary brain tumour for which there is no treatment that ensures long-term survival. Patients diagnosed with the most common adult form of this tumour, glioblastoma, survive on average only 14 months1. Symptoms usually occur only three months before diagnosis2; it is therefore important that indicators of the preclinical tumour be identified before the onset of symptoms.
Diabetes is a metabolic disease resulting from defects in insulin production leading to the inability of cells to use glucose and thus to elevated blood glucose levels. Although diabetes appears to increase the risk of most malignant tumours3, 11 out of 16 previous studies (e.g. refs 4,5,6,7) found an inverse association between diabetes and glioma or all types of brain tumours. A recent meta-analysis8 confirmed this inverse relationship. However, a recent cohort study of pre-diagnostic diabetes and cancer at all sites, in 2.3 million Israeli adults9, found an increased risk of malignant brain tumours among people diagnosed with diabetes.
People with diabetes may be diagnosed at different times during the course of the disease and this diagnosis is usually followed by treatments that may affect associations with subsequent glioma risk. We therefore focus the present study on associations between pre-diagnostic blood glucose levels and glioma risk as blood glucose levels may be measured routinely and are not necessarily followed by treatment. There are two previous studies reporting inverse associations between pre-diagnostic circulating glucose levels and glioma risk7, 10. Our study differs from this previous work because we concentrate on pre-diagnostic blood glucose and evaluate interactions between its levels and time from blood collection to brain tumour diagnosis and age at brain tumour diagnosis. In addition, we examined our data for the presence of competing risks.
Our reason for estimating the modifying effects of time before tumour diagnosis is as follows. If the nascent glioma is responsible for the association between blood glucose level and glioma, we would expect this association to vary with the proximity of blood collection to time of glioma diagnosis. Specifically, we propose that elevated consumption of blood glucose by the preclinical tumour may account for the apparent reduction of glioma risk among people with diabetes or elevated blood glucose levels. Cancer cells generate energy using aerobic glycolysis rather than oxidative phosphorylation used by non-proliferating cells. Aerobic glycolysis is less efficient than oxidative phosphorylation generating only two ATPs per molecule of glucose while oxidative phosphorylation generates 36 ATPs. Therefore, in general, cancer cells require more glucose than do non-proliferating cells. This phenomenon was first reported by Otto Warburg and is therefore referred to as the Warburg effect11. There is evidence of aerobic glycolysis in glioma12,13,14,15. Possibly consistent with this increased need for glucose, Seyfried et al.16 show that growth of astrocytoma in a mouse model is a direct function of blood glucose levels. Sturrock et al.17 developed a mathematical model describing this process. If the preclinical tumour reduces circulating blood glucose levels then one would expect an inverse association to be strongest near the time of glioma diagnosis17.
Our rationale for evaluating age at diagnosis as a modifying factor is based on results of a previous AMORIS study of pre-diagnostic serum glucose levels and prostate cancer risk18. In this study, Van Hemelrijck et al. found that the inverse association between blood glucose levels and prostate cancer diagnosis may be attributable, in part, to the phenomenon of competing risks19. That is, because elevated blood glucose levels increase the risk of death from both cardiovascular disease20 and cancer21, people with hyperglycaemia (≥5.6 mmol/L) would be expected to have higher all-cause mortality rates than would people with normal blood glucose levels. Thus people with hyperglycaemia are selected out of the population at risk of glioma making etiological inferences based on comparisons of the prevalence of hyperglycaemia between people with and without glioma invalid. To determine whether this potential source of selection bias is present, we estimated the modifying effects of age at diagnosis on the association between blood glucose levels and glioma. Competing risk bias would be expected to increase with age as do all-cause mortality rates. To further evaluate our data for the presence of competing risks, we used the sub-distribution hazards model22, 23 which is a more formal method of identifying competing risks.
Results
In Table 1 the relative proportions of male and female total glioma cases differ between the cohorts (in AMORIS 65% are men; in Me-Can 52%) as does fasting status (in AMORIS 61% of blood was drawn when total glioma cases were fasting; in Me-Can all blood samples were collected from fasting participants). The remaining descriptive characteristics of both high grade glioma (anaplastic astrocytoma and glioblastoma) and total glioma in the two cohorts are similar. For example, ages at the time of the initial blood test and the time of total glioma diagnosis are almost the same among total glioma patients in the two cohorts (AMORIS: ages 50 and 57 years respectively; Me-Can: ages 50 and 58 years, respectively) resulting in the same median periods of observation among cases (seven years) in both cohorts. Although non-cases have a longer median observation time in the AMORIS (15 years) than in the Me-Can cohort (12 years), total glioma incidence rates are similar. The incidence rate in the AMORIS cohort is 7.6/100,000 person years, while that in the Me-Can cohort is 6.4/100,000 person years.
Hazard ratios and trend test P-values in Table 2 are also similar for both sexes combined in the AMORIS and Me-Can cohorts, although these P-values primarily reflect the hazard ratios of the highest level of glucose (≥6.1 mmol/L) (AMORIS HR = 0.59, 95% CI 0.42 to 0.84; Me-Can HR = 0.58, 95% CI 0.32 to 1.04). Results restricted to high grade glioma (anaplastic astrocytoma and glioblastoma; Supplemental Table 1) do not differ substantially from those in Table 2.
Hazard ratios and trend test P-values produced by the sub-distribution hazards models (Supplemental Table 2) in the AMORIS cohort, are similar to those in the standard Cox models (Table 2) thus providing no evidence of competing risks. However, in the Me-Can cohort while hazard ratios (Supplemental Table 2) are similar to those in Table 2, P-values differ slightly. Taken together, however, these results indicate that competing risks are probably not driving our findings.
Pre-diagnostic diabetes is strongly inversely associated with glioma in the AMORIS cohort, (HR = 0.30, 95% CI 0.17 to 0.63), although it is based on only 12 glioma cases (2.0% of total glioma cases), 11 of which were found among men. There were 39,404 people (7.5% of the total non-cases) diagnosed with diabetes among the non-cases, men accounted for 25,392 of these diagnoses. Information on pre-diagnostic diabetes diagnoses was not available for the Me-Can cohort.
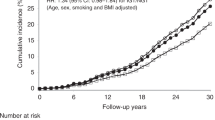
Table 3 shows hazard ratios by the time between the first blood glucose test and glioma diagnosis. These hazard ratios represent the change in the glioma hazard rate with a one unit change in blood glucose level. For example, among men whose blood was collected within the year before the end of follow-up, the hazard ratio based on the AMORIS data (HR = 0.78, 95% CI 0.65 to 0.94) indicates that glioma rates decrease 22% per unit increase of the standardised natural log of blood glucose. In addition, the trend test for both sexes combined indicates the presence of a linear trend (P trend = 0.04) over the levels of time before diagnosis. Thus the time of blood draw modifies the effect of glucose on the glioma rate, that is, there is a statistically significant interaction between time and glucose. There is no evidence of a similar effect of time before diagnosis in the Me-Can cohort. In addition, in an exploratory analysis of within-person time trends in 51 Me-Can patients with multiple blood glucose measurements, we found no trends by year before glioma diagnosis.
Age at glioma diagnosis (Table 4) significantly (P < 0.05) modifies the association between glucose and glioma risk among men older than age 70 years in the Me-Can cohort (Table 4, Me-Can: HR = 0.50, 95% CI 0.29 to 0.85), but does not in the AMORIS cohort (AMORIS: HR = 0.84, 95% CI 0.64 to 1.11). Age trends are of borderline statistical significance.
Discussion
We found inverse associations between pre-diagnostic blood glucose levels and glioma risk in both the AMORIS and Me-Can cohorts, and between diabetes and glioma in the AMORIS cohort. This blood glucose - glioma association was modified by time between the first blood glucose test and glioma diagnosis in the AMORIS cohort and possibly by age at glioma diagnosis in the Me-Can cohort. In addition, we found no evidence of competing risks.
Our blood glucose dose-response findings are similar to those reported for high grade and total glioma by Edlinger et al.10, using four additional sub-cohorts of the Me-Can study, and by Seliger et al.7. The inverse association between diabetes and glioma, in the AMORIS cohort, is also consistent with the majority of the previous literature7, 8.
The initial examination of the time and age interactions was hypothesis driven, as noted in the introduction, rather than based on statistical significance alone (see Statistical methods). In addition, the initial significance tests reflected the statistical significance of a single interaction term (stratified on the second time-related term). These tests are not as meaningful as the interaction analyses presented in Tables 3 and 4 because they mask time and age-specific trends. The significant and borderline significant trends in these tables show time interactions in the AMORIS cohort and age interactions in both cohorts. As described in the introduction, both time and age interactions may represent biologically meaningful effects. To assess their validity, these results require confirmation in subsequent studies.
The sub-distribution hazards model indicates the absence of competing risks; however, the weakness of this analytic approach is that although people who die are retained in risk sets after their deaths, the number of people diagnosed with glioma remains the same22, 23. Given this limitation, the strong inverse age-blood glucose association among people older than age 70 years in the Me-Can cohort may indicate the presence of competing risks from hyperglycaemia-associated deaths. However if our findings are attributable to competing risks one would expect the inverse diabetes-cancer relationship to be observed at cancer sites other than glioma. In fact, we see the opposite pattern. Tumours at most sites are positively associated with blood glucose level3, 24,25,26 with the known exceptions of meningioma in one study27 but not in another9 and prostate cancer18, 28.
Limitations of our study include the lack of sufficient information on body mass index, blood pressure and high and low density lipoprotein in the AMORIS cohort to include these variables in our regression models. These variables are associated with both diabetes29 and glioma10 and therefore qualify as potentially confounding variables. Also, there are several differences between the AMORIS and Me-Can cohorts that may affect comparisons. Serum glucose was measured in the AMORIS cohort while plasma glucose was measured in the Me-Can cohort. However Frank et al.30 found no physiologically relevant differences between these two methods of measuring circulating glucose. Another difference between these cohorts is that non-fasting serum glucose values were included in the AMORIS cohort but were not included in the Me-Can cohort although fasting and non-fasting glucose values in the AMORIS cohort were similar. In addition, Me-Can study participants were censored after diagnosis of any malignant tumour while AMORIS cohort participants were not. Despite these differences, cohort dose-response findings for the two cohorts are remarkably similar. Whether conflicting estimates of time and age interactions with blood glucose levels produced by the two cohorts are attributable to their differences in design is not known.
There are several potential mechanisms accounting for the inverse association between hyperglycaemia and glioma. The commonly prescribed anti-diabetic medication, metformin, inhibits glioblastoma cell proliferation and migration31 and may therefore reduce glioma risk. However, a large case-control study found no clear evidence of this association7.
Adverse effects of hyperglycaemia and diabetes that may paradoxically reduce glioma risk include diabetes-related reduction of bioavailable testosterone levels7, 32. Another possibility is the fact that both impaired glucose tolerance33 and diabetes34,35,36 lead to the shortening of telomeres (that is, the region at each end of a chromosome which prevents deterioration but shortens with each cell replication). The highest glioma risk alleles near the TERC and TERT gene are associated with long telomeres37 thus providing a potential rationale for our findings. The problem with this line of reasoning, however, is that one would expect hyperglycaemia to be inversely related to malignant melanoma, the risk of which is also positively associated with telomere length38, but it is not39.
Hyperglycaemia induces apoptosis and inhibits progression of neural stem cells40. To the extent that glioblastoma stem cells are related to neural stem cells41 hyperglycaemia may confer protection against glioblastoma. Another potential mechanism is inhibition of cerebral circulation associated with diabetes42, 43 causing reduced glioma risk44. In addition, lower levels of insulin-like growth factor 1 (IGF-1) are found in diabetic than in non-diabetic serum45 and tumour-associated macrophage derived IGF-1 may drive glioma recurrence46. These proposed mechanisms may work together or separately.
Overall, our findings provide further evidence of an inverse association between hyperglycaemia, diabetes and glioma. In contrast, evidence for the presence of the Warburg effect11 was mixed with the AMORIS data suggesting an inverse association during the year before glioma diagnosis and the Me-Can data showing no such association. Further investigation of a pre-diagnostic Warburg effect would be worthwhile, as would examination of associations between blood glucose level and glioma by genetic subtypes of type 2 diabetes47 and glioma48.
Methods
The AMORIS and Me-Can cohorts have been described in detail elsewhere49,50,51. Here we briefly summarise this information.
AMORIS cohort
This Swedish cohort links records from the Central Automation Laboratory (CALAB, Stockholm, Sweden) database (1985–1996) to those of the National Cancer Registry, the National Patient Register, the Cause of Death Register, and the National Register of Emigration. Endpoint ascertainment is based on the Swedish National Cancer Registry and therefore includes all glioma diagnoses among Swedish residents. Outcome data used in the present analyses are current as of December 31st, 2011.
The AMORIS cohort consists of 812,073 participants of all ages with 529,123 having been tested for serum glucose during their first lab visit. People under age 18 years old at the time of glioma diagnosis (event of interest) or death, emigration, or the end of follow-up (outcomes leading to censoring) were excluded from the study as their tumours may differ from those found in adults52. We then excluded 528 people diagnosed with meningioma (defined by pathology-anatomy diagnosis (PAD) codes (WHO/HS/CANC/24.1, Histology Code) 461 and 466) and 15 with ependymoma (PAD codes 481, 485). These additional exclusions reduced the sample to 528,580 participants, 604 of whom were subsequently diagnosed with glioma (PAD codes 475 (n = 128) and 476 (n = 476) and the International Classification of Disease 7th Edition (ICD-7) code 193) (see Supplemental Table 3). This project has been approved by the Regional Ethical committee at the Karolinska Institutet, Stockholm, Sweden (Registration number 2010/1:7). All the study data were de-identified and the ethical committee approved the project without collecting any additional informed consent. The project complied with the requirements of the Declaration of Helsinki.
Information on diabetes in the AMORIS cohort was based on the National Diabetes Register53 established in 1996 and the National Patient Register which began including outpatient diagnoses in 2001. The AMORIS study began in 1985 and the data set used in the present study ended in 2011 so information on diabetes was not complete, but presumably equally incomplete for glioma cases and non-cases. To partially address the absence of information on diabetes before 1996, we also classified individuals in our sample as diabetics if they had fasting serum glucose levels ≥ 7.0 mmol/L.
Me-Can cohort
Seven population-based sub-cohorts were originally included in the Me-Can study, however in the present investigation we used data from only the Austrian and the two Swedish sub-cohorts51. In brief, these sub-cohorts contained data on 269,365 participants, ranging from 19 to 96 years of age at baseline (between 1974 and 2005) without a known tumour, after exclusion of 2,711 non-fasting participants. Data included measured height, weight and blood pressure, as well as levels of fasting plasma glucose, triglycerides and total cholesterol. For this study, each individual’s baseline data were taken from the first (or only) health examination with complete or near-complete data. Nationwide cancer and cause-of-death registries were used to follow participants. Glioma diagnoses were based on PAD codes 475 (n = 21) and 476 (n = 96) and ICD-7 193 codes in the Swedish sub-cohorts. In the Austrian sub-cohort these diagnoses were identified using ICD-7 193 and histology codes 93803, 93813, 93823, 94003, 94013, 94113, 94203, 94213, 94403, 94503, and 94513 from ICD-O1 (see Supplemental Table 3). In this sub-cohort meningioma cases were not identified and are thus included among the non-cases. Ascertainment of endpoints in the Swedish sub-cohorts is based on the Swedish Cancer Registry and is complete. The Austrian sub-cohort is regularly linked to the regional cancer registry with high coverage and completeness. The study was approved by The Research Review Board of Umeå, Sweden, the Regional Committee for Medical and Health Research Ethics and the Ethikkommission of the Land Vorarlberg, Austria. Participants in Sweden and in Austria provided written informed consent to participate in the studies. All study data were de-identified.
The association between blood glucose and glioma risk has been previously reported using all seven population-based Me-Can sub-cohorts10 (we use only three of these in the present study). Here the exposure categories are different to allow comparison with the AMORIS cohort. More importantly, we evaluated time and age interactions and competing risks, which were not examined previously. Also, an exploratory analysis was performed using a subgroup with repeated exposure measurements.
Statistical methods
In our multivariable time-dependent Cox regression models, study participants were included in the analysis at their age at the time of their first blood glucose test (left-truncation) and exited the analysis at the age they were diagnosed with glioma or died, emigrated or when follow-up ended (whichever event came first). In addition, in the Me-Can cohort participants were also censored at the time of diagnosis of any malignant tumour. Follow-up time was restricted to a maximum of 15 years from the initial blood glucose test because we were interested in the hypothetical effect of the preclinical tumour on glucose levels (reverse causality) as well as the possible effects of blood glucose levels on glioma risk.
In the initial glucose dose-response analysis the first three lower cut points for the blood glucose variable were based on those in a previous paper using AMORIS cohort data18, the lowest cut point for the fourth glucose level (5.6 mmol/L) is, according to the American Diabetes Association54, the lowest level of blood glucose that indicates pre-diabetes, while the lower cut point for the fifth glucose level (6.1 mmol/L) is the lowest blood glucose value designated by the World Health Organization as an indication of impaired fasting glucose55. We used these cut points rather than quintiles because of their clinical significance.
Our time- dependent Cox regression models were adjusted for age at the time of the first blood glucose test, date at the time of the blood glucose test, fasting status, triglycerides, cholesterol levels, and gender. Using data from the AMORIS cohort, we found that when characterised by a single interaction term and stratified on the other time-related variable, the association between blood glucose and glioma varied with the time of the blood draw before glioma diagnosis (HR = 0.98, 95% CI = 0.96 to 1.00, P = 0.03) and age at glioma diagnosis (HR = 1.00, 95% CI = 1.00 to 1.01, P = 0.11). We therefore used the strata statement in PROC PHREG (SAS, version 9.4) and stratified these regression models by both time before diagnosis and age at diagnosis thus producing separate baseline hazards for each time and age-specific stratum56. For consistency, the Me-Can data were also stratified by sub-cohort, but not adjusted for fasting status since the few non-fasting participants were not included in the data set. We tested dose-response trends over time and age using linear contrasts, analysis of variance, and F-tests57.
In addition to estimating the overall association between blood glucose level and glioma, accounting for the modifying effects of time and age, we also estimated these time-related effects. As noted in the introduction above, these analyses were driven by theory, in addition to the initial statistical significance of the time-glioma interaction and borderline significance of the age interaction in the AMORIS data. Instead of using five categories of blood glucose, as we did in the dose-response Cox regression models, we analysed blood glucose level as a continuous variable within each of four categories of years before glioma diagnosis (≤1, 1–<5, 5–<10, 10–<15) and four categories of age in years at glioma diagnosis (≤50, >50–≤60, >60–≤70, >70). To avoid multicollinearity, we used two separate time-dependent Cox regression models; one representing time interactions and a second representing age interactions. To address the potential problem of the influence of outliers on the results, we used natural logarithms of the blood glucose values and standardised them to a mean of zero and a standard deviation of one. In addition, we accounted for that time-related variable which was not included in the model using the strata statement in PROC PHREG (SAS, version 9.4).
All Me-Can cohort study participants fasted before their blood was drawn; however only 56% of the AMORIS study participants did so. We therefore analysed AMORIS glucose dose-response relationships separately by fasting status. We found that fasting and non-fasting glucose dose-response relationships were similar (Supplemental Table 4) allowing us to combine data from these two groups.
Using the Me-Can data set, we conducted an exploratory analysis of the 51 glioma cases with multiple measurements to determine whether glucose values ≤7.0 mmol/L varied with the number of measurements or time between the blood glucose test and glioma diagnosis.
To find out whether competing risks affected our findings, in addition to estimating the potentially modifying effects of age at glioma diagnosis on the blood glucose-glioma association, we used the sub-distribution hazards regression model (SAS, version 9.4). Hazard ratios based on the latter model are those which would have been found had individuals who were at risk of glioma when they died remained in the population but were not subsequently diagnosed with glioma22, 23.
All analyses were conducted using SAS statistical software, version 9.4 (SAS Institute Inc, Cary, NC).
References
Johnson, D. R. & O’Neill, B. P. Glioblastoma survival in the United States before and during the temozolomide era. J Neurooncol. 107, 359–364, doi:10.1007/s11060-011-0749-4 (2012).
Ohgaki, H., Burger, P. & Kleihues, P. Definition of primary and secondary glioblastoma–response. Clin Cancer Res 20, 2013–2013, doi:10.1158/1078-0432.CCR-14-0238 (2014).
Giovannucci, E. et al. Diabetes and cancer: a consensus report. Diabetes Care. 33, 1674–1685, doi:10.2337/dc10-0666 (2010).
Cahoon, E. K., Inskip, P. D., Gridley, G. & Brenner, A. V. Immune-related conditions and subsequent risk of brain cancer in a cohort of 4.5 million male US veterans. Br J Cancer. 110, 1825–1833, doi:10.1038/bjc.2014.97 (2014).
Kitahara, C. M. et al. Personal history of diabetes, genetic susceptibility to diabetes, and risk of brain glioma: a pooled analysis of observational studies. Cancer Epidemiol Biomarkers Prev. 23, 47–54, doi:10.1158/1055-9965.EPI-13-0913 (2014).
Schwartzbaum, J. et al. Prior hospitalization for epilepsy, diabetes, and stroke and subsequent glioma and meningioma risk. Cancer Epidemiol Biomarkers Prev. 14, 643–650, doi:10.1158/1055-9965.EPI-04-0119 (2005).
Seliger, C. et al. Diabetes, use of antidiabetic drugs, and the risk of glioma. Neuro Oncol. 18, 340–349, doi:10.1093/neuonc/nov100 (2016).
Zhao, L., Zheng, Z. & Huang, P. Diabetes mellitus and the risk of glioma: a meta-analysis. Oncotarget. 7, 4483–4489, doi:10.18632/oncotarget.6605 (2016).
Dankner, R. et al. Time-dependent risk of cancer after a diabetes diagnosis in a cohort of 2.3 million adults. Am J Epidemiol. 183, 1098–1106, doi:10.1093/aje/kwv290 (2016).
Edlinger, M. et al. Blood pressure and other metabolic syndrome factors and risk of brain tumour in the large population-based Me-Can cohort study. J Hypertens. 30, 290–296, doi:10.1097/HJH.0b013e32834e9176 (2012).
Vander Heiden, M. G., Cantley, L. C. & Thompson, C. B. Understanding the Warburg effect: the metabolic requirements of cell proliferation. Science. 324, 1029–1033, doi:10.1126/science.1160809 (2009).
Purow, B. For glioma, a sweet side to diabetes. Neuro Oncol. 18, 306–307, doi:10.1093/neuonc/nov328 (2016).
Nie, Q. et al. Overexpression of isocitrate dehydrogenase-1R132H enhances the proliferation of A172 glioma cells via aerobic glycolysis. Mol Med Rep. 11, 3715–3721, doi:10.3892/mmr.2015.3187 (2015).
Marin-Valencia, I. et al. Analysis of tumor metabolism reveals mitochondrial glucose oxidation in genetically diverse human glioblastomas in the mouse brain in vivo. Cell Metab. 15, 827–837, doi:10.1016/j.cmet.2012.05.001 (2012).
Mao, P. et al. Mesenchymal glioma stem cells are maintained by activated glycolytic metabolism involving aldehyde dehydrogenase 1A3. Proc Natl Acad Sci USA 110, 8644–8649, doi:10.1073/pnas.1221478110 (2013).
Seyfried, T. N., Sanderson, T. M., El-Abbadi, M. M., McGowan, R. & Mukherjee, P. Role of glucose and ketone bodies in the metabolic control of experimental brain cancer. Br J Cancer 89, 1375–1382, doi:10.1038/sj.bjc.6601269 (2003).
Sturrock, M., Hao, W., Schwartzbaum, J. & Rempala, G. A. A mathematical model of pre-diagnostic glioma growth. J Theor Biol. 380, 299–308, doi:10.1016/j.jtbi.2015.06.003 (2015).
Van Hemelrijck, M. et al. Prostate cancer risk in the Swedish AMORIS study: the interplay among triglycerides, total cholesterol, and glucose. Cancer. 117, 2086–2095, doi:10.1002/cncr.25758 (2011).
Häggström, C. et al. Interpretation of conventional survival analysis and competing-risk analysis: an example of hypertension and prostate cancer. BJU Int. 118, 850–852, doi:10.1111/bju.2016.118.issue-6 (2016).
Davidson, J. A. & Parkin, C. G. Is hyperglycemia a causal factor in cardiovascular disease? Does proving this relationship really matter? Yes. Diabetes Care. 32(Suppl 2), S331–333, doi:10.2337/dc09-S333 (2009).
Ryu, T. Y., Park, J. & Scherer, P. E. Hyperglycemia as a risk factor for cancer progression. Diabetes Metab. 38, 330–336, doi:10.4093/dmj.2014.38.5.330 (2014).
Fine, J. P. & Gray, R. J. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 94, 496–509, doi:10.1080/01621459.1999.10474144 (1999).
Lau, B., Cole, S. R. & Gange, S. J. Competing risk regression models for epidemiologic data. Am J Epidemiol. 170, 244–256, doi:10.1093/aje/kwp107 (2009).
Bosco, C. et al. Metabolic serum biomarkers for the prediction of cancer: a follow-up of the studies conducted in the Swedish AMORIS study. Ecancermedicalscience. 9, 555, doi:10.3332/ecancer.2015.555 (2015).
Stocks, T. et al. Metabolic risk score and cancer risk: pooled analysis of seven cohorts. Int J Epidemiol. 44, 1353–1363, doi:10.1093/ije/dyv001 (2015).
Stocks, T. et al. Blood glucose and risk of incident and fatal cancer in the metabolic syndrome and cancer project (me-can): analysis of six prospective cohorts. PLoS Med. 6, e1000201, doi:10.1371/journal.pmed.1000201 (2009).
Bernardo, B. M. et al. Association between prediagnostic glucose, triglycerides, cholesterol and meningioma, and reverse causality. Br J Cancer. 115, 108–114, doi:10.1038/bjc.2016.157 (2016).
Häggström, C. et al. Prostate cancer, prostate cancer death, and death from other causes, among men with metabolic aberrations. Epidemiology. 25, 823–828, doi:10.1097/EDE.0000000000000174 (2014).
Healy, G. N. et al. Objectively measured sedentary time, physical activity, and metabolic risk: the Australian diabetes, obesity and lifestyle study (AusDiab). Diabetes Care. 31, 369–371, doi:10.2337/dc07-1795 (2008).
Frank, E. A., Shubha, M. C. & D’Souza, C. J. Blood glucose determination: plasma or serum? J Clin Lab Anal. 26, 317–320, doi:10.1002/jcla.21524 (2012).
Seliger, C. et al. Metformin inhibits proliferation and migration of glioblastoma cells independently of TGF-β2. Cell Cycle. 15, 1755–1766, doi:10.1080/15384101.2016.1186316 (2016).
Rao, P. M., Kelly, D. M. & Jones, T. H. Testosterone and insulin resistance in the metabolic syndrome and T2DM in men. Nat Rev Endocrinol. 9, 479–493, doi:10.1038/nrendo.2013.122 (2013).
Adaikalakoteswari, A., Balasubramanyam, M., Ravikumar, R., Deepa, R. & Mohan, V. Association of telomere shortening with impaired glucose tolerance and diabetic macroangiopathy. Atherosclerosis. 195, 83–89, doi:10.1016/j.atherosclerosis.2006.12.003 (2007).
Zhou, Y., Ning, Z., Lee, Y., Hambly, B. D. & McLachlan, C. S. Shortened leukocyte telomere length in type 2 diabetes mellitus: genetic polymorphisms in mitochondrial uncoupling proteins and telomeric pathways. Clin Transl Med. 5, 8, doi:10.1186/s40169-016-0089-2 (2016).
Tamura, Y., Takubo, K., Aida, J., Araki, A. & Ito, H. Telomere attrition and diabetes mellitus. Geriatr Gerontol Int. 16(Suppl 1), 66–74, doi:10.1111/ggi.2016.16.issue-s1 (2016).
Masi, S. et al. Telomere length, antioxidant status and incidence of ischaemic heart disease in type 2 diabetes. Int J Cardiol. 216, 159–164, doi:10.1016/j.ijcard.2016.04.130 (2016).
Walsh, K. M., Ohgaki, H. & Wrensch, M. R. Epidemiology. Handb Clin Neurol. 134, 3–18, doi:10.1016/B978-0-12-802997-8.00001-3 (2016).
Nan, H. et al. Shorter telomeres associate with a reduced risk of melanoma development. Cancer Res. 71, 6758–6763, doi:10.1158/0008-5472.CAN-11-1988 (2011).
Qi, L. et al. Type 2 diabetes mellitus and risk of malignant melanoma: a systematic review and meta-analysis of cohort studies. Iran J Public Health. 43, 857–866 (2014).
Chen, J. et al. High glucose induces apoptosis and suppresses proliferation of adult rat neural stem cells following in vitro ischemia. BMC Neurosci. 14, 24, doi:10.1186/1471-2202-14-24 (2013).
Goffart, N., Kroonen, J. & Rogister, B. Glioblastoma-initiating cells: relationship with neural stem cells and the micro-environment. Cancers (Basel) 5, (1049–1071 (2013).
Chung, C. C. et al. Inflammation-associated declines in cerebral vasoreactivity and cognition in type 2 diabetes. Neurology. 85, 450–458, doi:10.1212/WNL.0000000000001820 (2015).
Rusinek, H. et al. Cerebral perfusion in insulin resistance and type 2 diabetes. J Cereb Blood Flow Metab. 35, 95–102, doi:10.1038/jcbfm.2014.173 (2015).
Letourneur, A. et al. Chronic arterial hypertension impedes glioma growth: a multiparametric MRI study in the rat. Hypertens Res. 38, 723–732, doi:10.1038/hr.2015.66 (2015).
Teppala, S. & Shankar, A. Association between serum IGF-1 and diabetes among U.S. adults. Diabetes Care. 33, 2257–2259, doi:10.2337/dc10-0770 (2010).
Quail, D. F. et al. The tumor microenvironment underlies acquired resistance to CSF-1R inhibition in gliomas. Science. 352, aad3018–aad3018, doi:10.1126/science.aad3018 (2016).
Flannick, J., Johansson, S. & Njølstad, P. R. Common and rare forms of diabetes mellitus: towards a continuum of diabetes subtypes. Nat Rev Endocrinol. 12, 394–406, doi:10.1038/nrendo.2016.50 (2016).
Eckel-Passow, J. E. et al. Glioma groups based on 1p/19q, IDH, and TERT promoter mutations in tumors. N Engl J Med. 372, 2499–2508, doi:10.1056/NEJMoa1407279 (2015).
Walldius, G. et al. High apolipoprotein B, low apolipoprotein A-I, and improvement in the prediction of fatal myocardial infarction (AMORIS study): a prospective study. Lancet. 358, 2026–2033, doi:10.1016/S0140-6736(01)07098-2 (2001).
Walldius, G., Jungner, I., Kolar, W., Holme, I. & Steiner, E. High cholesterol and triglyceride values in Swedish males and females: increased risk of fatal myocardial infarction. First report from the AMORIS (Apolipoprotein related MOrtality RISk) study. Blood Press Suppl. 4, 35–42 (1992).
Stocks, T. et al. Cohort profile: the Metabolic syndrome and Cancer project (Me-Can). Int J Epidemiol. 39, 660–667, doi:10.1093/ije/dyp186 (2010).
Paugh, B. S. et al. Integrated molecular genetic profiling of pediatric high-grade gliomas reveals key differences with the adult disease. J Clin Oncol. 28, 3061–3068, doi:10.1200/JCO.2009.26.7252 (2010).
Gudbjörnsdottir, S., Cederholm, J., Nilsson, P. M. & Eliasson, B. & Steering Committee of the Swedish National Diabetes Register. The National Diabetes Register in Sweden: an implementation of the St. Vincent declaration for quality improvement in diabetes care. Diabetes Care. 26, 1270–1276 (2003).
Gupta, A. K., Brashear, M. M. & Johnson, W. D. Prediabetes and prehypertension in healthy adults are associated with low vitamin D levels. Diabetes Care. 34, 658–660, doi:10.2337/dc10-1829 (2011).
Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care. 20, 1183–1197 (1997).
Borucka, J. Extensions of Cox model for non-proportional hazards purpose. Ekonometria 3, 85–101, doi:10.15611/ekt.2014.3 (2014).
Casella, G. Statistical Design. (Springer, 2008).
Acknowledgements
National Cancer Institute, National Institutes of Health (grant number R01CA122163) to J.S.
Author information
Authors and Affiliations
Contributions
J.S., M.E., G.A.R., H.U., H.M., and M.F. conceived study and designed analysis. M.E., P.S., G.N., N.K., B.F., and J.M. contributed data. J.S., M.E., V.Z., P.S., G.N., N.K., H.U., B.F., G.W., J.M., and M.F. wrote or revised manuscript. All authors read and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Schwartzbaum, J., Edlinger, M., Zigmont, V. et al. Associations between prediagnostic blood glucose levels, diabetes, and glioma. Sci Rep 7, 1436 (2017). https://doi.org/10.1038/s41598-017-01553-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-01553-2
This article is cited by
-
Therapeutic benefit of combining calorie-restricted ketogenic diet and glutamine targeting in late-stage experimental glioblastoma
Communications Biology (2019)
-
Provocative Question: Should Ketogenic Metabolic Therapy Become the Standard of Care for Glioblastoma?
Neurochemical Research (2019)
-
Searching for the roots of brain cancer
Nature (2018)
-
Influence of obesity-related risk factors in the aetiology of glioma
British Journal of Cancer (2018)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.