Abstract
Alzheimer’s disease (AD) is characterized by the spread of tau pathology throughout the cerebral cortex. This spreading pattern was thought to be fairly consistent across individuals, although recent work has demonstrated substantial variability in the population with AD. Using tau-positron emission tomography scans from 1,612 individuals, we identified 4 distinct spatiotemporal trajectories of tau pathology, ranging in prevalence from 18 to 33%. We replicated previously described limbic-predominant and medial temporal lobe-sparing patterns, while also discovering posterior and lateral temporal patterns resembling atypical clinical variants of AD. These ‘subtypes’ were stable during longitudinal follow-up and were replicated in a separate sample using a different radiotracer. The subtypes presented with distinct demographic and cognitive profiles and differing longitudinal outcomes. Additionally, network diffusion models implied that pathology originates and spreads through distinct corticolimbic networks in the different subtypes. Together, our results suggest that variation in tau pathology is common and systematic, perhaps warranting a re-examination of the notion of ‘typical AD’ and a revisiting of tau pathological staging.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Data availability
The tau PET data contributing to this study were sourced from six different cohorts. One of them, ADNI, is a public access dataset and can be obtained by application from http://adni.loni.usc.edu/. Data from the other datasets are not publicly available for download, but access requests can be made to the respective study investigators: BioFINDER 1,2—O.H.; UCSF Memory and Aging Center—G.D.R.; Gangnam Severance Hospital—C.H.L.; AVID Radiopharmaceuticals—M.J.P. and M.D.D. Additionally, the CMU-60 diffusion tensor imaging (DTI) data used to create the template DTI connectomes are publicly available and can be accessed at https://www.cmu.edu/dietrich/psychology/cognitiveaxon/data.html.
Code availability
Python and MATLAB implementations of the SuStaIn algorithm are available on the UCL-POND GitHub page: https://github.com/ucl-pond. The ESM algorithm is available for academics as part of open-access, user-friendly software (for further details, visit https://www.neuropm-lab.com/).
References
Hurd, M. D., Martorell, P., Delavande, A., Mullen, K. J. & Langa, K. M. Monetary costs of dementia in the United States. N. Engl. J. Med. 368, 1326–1334 (2013).
Alafuzoff, I. et al. Staging of neurofibrillary pathology in Alzheimer’s disease: a study of the BrainNet Europe Consortium. Brain Pathol. 18, 484–496 (2008).
Hyman, B. T. et al. National Institute on Aging—Alzheimer’s Association guidelines for the neuropathologic assessment of Alzheimer’s disease. Alzheimers Dement. 8, 1–13 (2012).
Hardy, J. & Selkoe, D. J. The amyloid hypothesis of Alzheimer’s disease: progress and problems on the road to therapeutics. Science 297, 353–356 (2002).
Jack, C. R. Jr et al. Tracking pathophysiological processes in Alzheimer’s disease: an updated hypothetical model of dynamic biomarkers. Lancet Neurol. 12, 207–216 (2013).
La Joie, R. et al. Prospective longitudinal atrophy in Alzheimer’s disease correlates with the intensity and topography of baseline tau-PET. Sci. Transl. Med. 12, eaau5732 (2020).
Bejanin, A. et al. Tau pathology and neurodegeneration contribute to cognitive impairment in Alzheimer’s disease. Brain 140, 3286–3300 (2017).
Braak, H. & Braak, E. Neuropathological stageing of Alzheimer-related changes. Acta Neuropathol. 82, 239–259 (1991).
Braak, H., Alafuzoff, I., Arzberger, T., Kretzschmar, H. & Del Tredici, K. Staging of Alzheimer disease-associated neurofibrillary pathology using paraffin sections and immunocytochemistry. Acta Neuropathol. 112, 389–404 (2006).
Schöll, M. et al. PET imaging of tau deposition in the aging human brain. Neuron 89, 971–982 (2016).
Schwarz, A. Regional profiles of the candidate tau PET ligand 18 F-AV-1451 recapitulate key features of Braak histopathological stages. Brain 139, 1539–1550 (2016).
Murray, M. E. et al. Neuropathologically defined subtypes of Alzheimer’s disease with distinct clinical characteristics: a retrospective study. Lancet Neurol. 10, 785–796 (2011).
Whitwell, J. L. et al. Neuroimaging correlates of pathologically defined subtypes of Alzheimer’s disease: a case-control study. Lancet Neurol. 11, 868–877 (2012).
Ferreira, D., Nordberg, A. & Westman, E. Biological subtypes of Alzheimer’s disease: a systematic review and meta-analysis. Neurology 94, 436–448 (2020).
Ossenkoppele, R. et al. Tau PET patterns mirror clinical and neuroanatomical variability in Alzheimer’s disease. Brain 139, 1551–1567 (2016).
Crutch, S. J. et al. Consensus classification of posterior cortical atrophy. Alzheimers Dement. 13, 870–884 (2017).
Gorno-Tempini, M. L. et al. Classification of primary progressive aphasia and its variants. Neurology 76, 1006–1014 (2011).
Ossenkoppele, R. et al. The behavioural/dysexecutive variant of Alzheimer’s disease: clinical, neuroimaging and pathological features. Brain 138, 2732–2749 (2015).
Drummond, E. et al. Proteomic differences in amyloid plaques in rapidly progressive and sporadic Alzheimer’s disease. Acta Neuropathol. 133, 933–954 (2017).
Crist, A. M. et al. Leveraging selective hippocampal vulnerability among Alzheimer’s disease subtypes reveals a novel tau binding partner SERPINA5. Preprint at bioRxiv https://doi.org/10.1101/2020.12.18.423469 (2020).
Risacher, S. L. et al. Alzheimer disease brain atrophy subtypes are associated with cognition and rate of decline. Neurology 89, 2176–2186 (2017).
Ossenkoppele, R. et al. Distinct tau PET patterns in atrophy‐defined subtypes of Alzheimer’s disease. Alzheimers Dement. 16, 335–344 (2020).
Young, A. L. et al. Uncovering the heterogeneity and temporal complexity of neurodegenerative diseases with Subtype and Stage Inference. Nat. Commun. 9, 4273 (2018).
Dong, A. et al. Heterogeneity of neuroanatomical patterns in prodromal Alzheimer’s disease: links to cognition, progression and biomarkers. Brain 140, 735–747 (2017).
Noh, Y. et al. Anatomical heterogeneity of Alzheimer disease: based on cortical thickness on MRIs. Neurology 83, 1936–1944 (2014).
Tam, A. et al. A highly predictive signature of cognition and brain atrophy for progression to Alzheimer’s dementia. Gigascience 8, giz055 (2019).
Vogel, J. W. et al. Data-driven approaches for tau-PET imaging biomarkers in Alzheimer’s disease. Hum. Brain Mapp. 40, 638–651 (2019).
Leuzy, A. et al. Diagnostic performance of RO948 F 18 tau positron emission tomography in the differentiation of Alzheimer disease from other neurodegenerative disorders. JAMA Neurol. 77, 955–965 (2020).
Vogel, J. W. et al. Spread of pathological tau proteins through communicating neurons in human Alzheimer’s disease. Nat. Commun. 11, 2612 (2020).
Marshall, G. A., Fairbanks, L. A., Tekin, S., Vinters, H. V. & Cummings, J. L. Early-onset Alzheimer’s disease is associated with greater pathologic burden. J. Geriatr. Psychiatry Neurol. 20, 29–33 (2007).
Whitwell, J. L. et al. The role of age on tau PET uptake and gray matter atrophy in atypical Alzheimer’s disease. Alzheimers Dement. 15, 675–685 (2019).
Pontecorvo, M. J. et al. A multicentre longitudinal study of flortaucipir (18F) in normal ageing, mild cognitive impairment and Alzheimer’s disease dementia. Brain 142, 1723–1735 (2019).
Jack, C. R. et al. Predicting future rates of tau accumulation on PET. Brain 143, 3136–3150 (2020).
La Joie, R. et al. Association of APOE4 and clinical variability in Alzheimer disease with the pattern of tau- and amyloid-PET. Neurology 96, e650–e661 (2021).
Dujardin, S. et al. Tau molecular diversity contributes to clinical heterogeneity in Alzheimer’s disease. Nat. Med. 26, 1256–1263 (2020).
Aoyagi, A. et al. Aβ and tau prion-like activities decline with longevity in the Alzheimer’s disease human brain. Sci. Transl. Med. 11, eaat8462 (2019).
Koedam, E. L. G. E. et al. Early-versus late-onset Alzheimer’s disease: more than age alone. J. Alzheimers Dis. 19, 1401–1408 (2010).
Sun, N., Mormino, E. C., Chen, J., Sabuncu, M. R. & Yeo, B. T. T. Multi-modal latent factor exploration of atrophy, cognitive and tau heterogeneity in Alzheimer’s disease. Neuroimage 201, 116043 (2019).
Franzmeier, N. et al. Patient-centered connectivity-based prediction of tau pathology spread in Alzheimer’s disease. Sci. Adv. 6, eabd1327 (2020).
Mukaetova-Ladinska, E. B. et al. Regional distribution of paired helical filaments and normal tau proteins in aging and in Alzheimer’s disease with and without occipital lobe involvement. Dement. Geriatr. Cogn. Disord. 3, 61–69 (1992).
McKee, A. C. et al. Visual association pathology in preclinical Alzheimer disease. J. Neuropathol. Exp. Neurol. 65, 621–630 (2006).
Pikkarainen, M., Kauppinen, T. & Alafuzoff, I. Hyperphosphorylated tau in the occipital cortex in aged nondemented subjects. J. Neuropathol. Exp. Neurol. 68, 653–660 (2009).
Hanna Al-Shaikh, F. S. et al. Selective vulnerability of the nucleus basalis of Meynert among neuropathologic subtypes of Alzheimer disease. JAMA Neurol. 77, 225–233 (2019).
Machado, A. et al. The cholinergic system in subtypes of Alzheimer’s disease: an in vivo longitudinal MRI study. Alzheimers Res. Ther. 12, 51 (2020).
Rogalski, E., Johnson, N., Weintraub, S. & Mesulam, M. Increased frequency of learning disability in patients with primary progressive aphasia and their first-degree relatives. Arch. Neurol. 65, 244–248 (2008).
Ossenkoppele, R. et al. Discriminative accuracy of [18F]flortaucipir positron emission tomography for Alzheimer disease vs other neurodegenerative disorders. JAMA 320, 1151–1162 (2018).
Miller, Z. A. Cortical developmental abnormalities in logopenic variant primary progressive aphasia with dyslexia. Brain Commun. 1, fcz027 (2019).
Hyman, B. T. Tau propagation, different tau phenotypes, and prion-like properties of tau. Neuron 82, 1189–1190 (2014).
He, Z. et al. Transmission of tauopathy strains is independent of their isoform composition. Nat. Commun. 11, 7 (2020).
Leng, K. et al. Molecular characterization of selectively vulnerable neurons in Alzheimer’s disease. Nat. Neurosci. 24, 276–287 (2021).
Lemoine, L., Leuzy, A., Chiotis, K., Rodriguez-Vieitez, E. & Nordberg, A. Tau positron emission tomography imaging in tauopathies: the added hurdle of off-target binding. Alzheimers Dement. (Amst.) 10, 232–236 (2018).
Baker, S. L., Harrison, T. M., Maaß, A., La Joie, R. & Jagust, W. Effect of off-target binding on 18 F-flortaucipir variability in healthy controls across the lifespan. J. Nucl. Med. https://doi.org/10.2967/jnumed.118.224113 (2019).
Smith, R. et al. Head-to-head comparison of tau positron emission tomography tracers [18F]flortaucipir and [18F]RO948. Eur. J. Nucl. Med. Mol. Imaging 47, 342–354 (2020).
Fleisher, A. S. et al. Positron emission tomography imaging with [18F]flortaucipir and postmortem assessment of Alzheimer disease neuropathologic changes. JAMA Neurol. 77, 829–839 (2020).
Lowe, V. J. et al. Tau-positron emission tomography correlates with neuropathology findings. Alzheimers Dement. 16, 561–571 (2020).
Soleimani-Meigooni, D. N. et al. 18F-flortaucipir PET to autopsy comparisons in Alzheimer’s disease and other neurodegenerative diseases. Brain 143, 3477–3494 (2020).
Smith, R., Wibom, M., Pawlik, D., Englund, E. & Hansson, O. Correlation of in vivo [18F]flortaucipir with postmortem Alzheimer disease Tau pathology. JAMA Neurol. 76, 310–317 (2019).
Cho, H. et al. Predicted sequence of cortical tau and amyloid-β deposition in Alzheimer disease spectrum. Neurobiol. Aging 68, 76–84 (2018).
Iturria-Medina, Y., Sotero, R. C., Toussaint, P. J. & Evans, A. C. Epidemic spreading model to characterize misfolded proteins propagation in aging and associated neurodegenerative disorders. PLoS Comput. Biol. 10, e1003956 (2014).
Craddock, C. et al. Towards automated analysis of connectomes: the configurable pipeline for the analysis of connectomes (C-PAC). Front. Neuroinform. https://doi.org/10.3389/conf.fninf.2014.08.00117 (2013).
Acknowledgements
The authors thank M. Chakravarty, B. Misic, P. Bellec, P. Rosa-Neto, A. Dagher, E. Hamel and W. Seeley for feedback during the composition of this manuscript. J.W.V. acknowledges support from the government of Canada through a tri-council Vanier Canada Graduate Doctoral fellowship from the McGill Centre for Integrative Neuroscience and the Healthy Brains, Healthy Lives initiative, and from the National Institutes of Health (NIH) (no. T32MH019112). A.L.Y. is supported by a Medical Research Council Skills Development Fellowship (MR/T027800/1). N.P.O. is a UK Research and Innovation Future Leaders Fellow (no. MR/S03546X/1). N.P.O. and D.C.A. acknowledge support from the UK National Institute for Health Research University College London Hospitals Biomedical Research Centre, and D.C.A. acknowledges support from the Engineering and Physical Sciences Research Council grant no. EP/M020533/1. M.J.G. is supported by the Miguel Servet program (no. CP19/00031) and a research grant (no. PI20/00613) of the Instituto de Salud Carlos III-Fondo Europeo de Desarrollo Regional. R.L.J. acknowledges support from the NIH (no. K99AG065501). This project received funding from the European Union’s Horizon 2020 research and innovation programme under grant no. 666992. The BioFINDER studies are supported by the Swedish Research Council (no. 2016-00906), the Knut and Alice Wallenberg Foundation (no. 2017-0383), the Marianne and Marcus Wallenberg Foundation (no. 2015.0125), the Strategic Research Area MultiPark (Multidisciplinary Research in Parkinson’s disease) at Lund University, the Swedish Alzheimer’s Foundation (no. AF-939932), the Swedish Brain Foundation (no. FO2019-0326), the Swedish Parkinson Foundation (no. 1280/20), the Skåne University Hospital Foundation (no. 2020-O000028), Regionalt Forskningsstöd (no. 2020-0314) and the Swedish Federal Government under the ALF agreement (no. 2018-Projekt0279). The Tau PET study in Gangnam Severance Hospital was supported by a grant from the Basic Science Research Program through the National Research Foundation of Korea funded by the Ministry of Education (nos. NRF2018R1D1A1B07049386 and NRF2020R1F1A1076154) and a grant from the Korea Health Technology R&D Project through the Korea Health Industry Development Institute funded by the Ministry of Health and Welfare, Republic of Korea (grant no. HI18C1159). We also thank B. L. Miller, H. J. Rosen, M. Gorno Tempini and W. Jagust for supporting the UCSF tau-PET studies, which were funded through the following sources: National Institute on Aging (NIA) no. R01 AG045611 (G.D.R.), no. P50 AG23501 (B.L.M., H.J.R., G.D.R.), no. P01 AG019724 (B.L.M., H.J.R., G.D.R.). The precursor of 18F-flortaucipir was provided by AVID Radiopharmaceuticals. The precursor of 18F-flutemetamol was sponsored by GE Healthcare. The precursor of 18F-RO948 was provided by Roche. Data collection and sharing for this project were funded by ADNI (NIH grant no. U01 AG024904) and Department of Defense ADNI (award no. W81XWH-12-2-0012). ADNI is funded by the NIA, the National Institute of Biomedical Imaging and Bioengineering and through generous contributions from the following: AbbVie, Alzheimer’s Association; Alzheimer’s Drug Discovery Foundation; Araclon Biotech; Bioclinica; Biogen; Bristol Myers Squibb; CereSpir; Cogstate; Eisai; Elan Pharmaceuticals; Eli Lilly and Company; EUROIMMUN; F. Hoffmann-La Roche and its affiliated company Genentech; Fujirebio; GE Healthcare; IXICO; Janssen Alzheimer Immunotherapy Research Development; Johnson & Johnson Pharmaceutical Research Development; Lumosity; Lundbeck; Merck; Meso Scale Diagnostics; NeuroRx Research; Neurotrack Technologies; Novartis Pharmaceuticals Corporation; Pfizer; Piramal Imaging; Servier; Takeda Pharmaceutical Company; and Transition Therapeutics. The Canadian Institutes of Health Research is providing funds to support ADNI clinical sites in Canada. Private sector contributions are facilitated by the Foundation for the National Institutes of Health (www.fnih.org). The grantee organization is the Northern California Institute for Research and Education, and the study is coordinated by the Alzheimer’s Therapeutic Research Institute at the University of Southern California. ADNI data are disseminated by the Laboratory for Neuro Imaging at the University of Southern California. Finally, we thank all participants of this study and the families and caregivers of the patients included for their support in volunteering data for this study. Data used in the preparation of this article were obtained from the Alzheimer’s Disease Neuroimaging Initiative (ADNI) database (http://adni.loni.usc.edu/). As such, the investigators within the ADNI contributed to the design and implementation of ADNI and/or provided data but did not participate in analysis or writing of this report.
Author information
Authors and Affiliations
Consortia
Contributions
J.W.V., O.H. and A.C.E. conceptualized the work. J.W.V., A.L.Y., N.P.O., L.M.A., M.J.P., M.J.G and O.H. contributed to the analytical design. M.J.P., M.D.D., G.D.R., C.H.L. and O.H. acquired and provided the data. R.S., R.O., O.T.S. and R.L.J. contributed to data curation and processing. J.W.V. analyzed the data. A.L.Y. and D.C.A. originally created the SuStaIn algorithm, and N.P.O. and L.M.A. contributed to its execution. Y.I.M. created the ESM algorithm. J.W.V. and O.H. drafted the manuscript. All authors interpreted the data and contributed substantively to revising the manuscript.
Corresponding authors
Ethics declarations
Competing interests
M.J.P. and M.D.D. are employees of AVID Radiopharmaceuticals, a wholly owned subsidiary of Eli Lilly and Company, and are minor stockholders in Eli Lilly and Company. O.H. has acquired research support (for the institution) from AVID Radiopharmaceuticals, Biogen, Eli Lilly and Company, Eisai, GE Healthcare, Pfizer and Roche. In the past two years, he has received consultancy/speaker fees from AC Immune, ALZpath, Biogen, Cerveau and Roche. The remaining authors declare no competing interests.
Additional information
Peer reviewer information Nature Medicine thanks Giovanni Frisoni and the other, anonymous, reviewer(s), for their contribution to the peer review of this work. Jerome Staal was the primary editor on this article and managed its editorial process and peer review in collaboration with the rest of the editorial team.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Methodological details.
Methodological details. a, SuStaIn requires both spatial (for example brain regions) and pseudotemporal (for example Z-score waypoints representing advancing biomarker severity) features as input. SuStaIn models linear change between waypoints across multiple biomarkers and uses clustering to fit subtype trajectories representing distinct biomarker sequences. b, Each spatial feature was z-scored in order to derive interpretable waypoints. Example: (top left), SUVR distribution in the left temporal lobe. (bottom-left) Distribution of standardized residuals after regression of choroid plexus. Gaussian mixture-modeling identifies ‘normal’ (grey) and ‘abnormal’ (red) tau-PET values within this distribution. (bottom right) Mean and SD of ‘normal’ distribution used to normalize the whole distribution, creating ‘Tau Z-scores’. Tau Z-scores of 2, 5 and 10 are used as waypoints. (top-right) Tau-z scores superimposed onto the original SUVR distribution. For each subtype model (k = 1-7), c) distribution of average negative log-likelihood, d) CVIC, and e) distribution of the probability of the maximum-likelihood subtype across cross-validation folds of left-out individuals. Higher log-likelihood, lower CVIC represents better model fit. f, Visualization of subtype solutions k = 2-7. For each subtype, the rendered brains show significant regional tau difference between the subtype and all other subtypes in its solution. Connecting-line thickness indicates how many subjects are shared between a subtype and each subtype from its parent and child solutions. Circle color represents which k = 4 subtypes (outlined in the dashed box) each subtype is most similar to, in terms of the number of overlapping subjects. Red arrowheads indicate subtypes that were formed by pooling individuals from two different parent subtypes. For boxplots in c,e, center line=median, box=inner quartiles, whiskers=extent of data distribution except *=outliers.
Extended Data Fig. 2 Details of subtype assignment.
Details of subtype assignment. a, Several individuals classified as S2 (MTL-Sparing) were found to be tau-negative (that is no significant tau in the entorhinal cortex or precuneus; S2: False). Cortical rendering shows the overall mean tau Z-scores (see Extended Data Fig. 1b) of S2: False individuals. Slightly elevated signal was observed throughout the cortex (but not MTL areas), including in regions where pathological tau is not typically observed until late AD. b, Proportion of Ab + (top) and cognitively impaired (bottom) individuals in S2: False (n = 54) compared to other S2 individuals (S2: True, n = 79) and tau-negative individuals (S0, n = 646). Using, χ2-tests with Tukey’s posthoc correction, a higher proportion of S2: False and S0 individuals were Aβ- (S0 p[adj]=8.5e-13; S2:F p[adj]=9.7e-08) and cognitively unimpaired (S0 p[adj]=6.2e-68; S2:F p[adj]=2.0e-10) than S2: True individuals, but did not differ significantly from one another (Ab p[adj]=0.94; cog p[adj]=0.07). c, Using two-sided ANOVAs with Tukey’s posthoc correction, S0 and S2: False individuals were older (S0 p[adj]=0.001; S2:F p([adj]=0.024) and had higher MMSE scores (S0 adj]=0.001; S2:F p([adj]=0.001) than S2: True individuals, but did not differ from one another (Age p[adj]=0.48; MMSE p[adj]=0.21). d, SuStaIn stage of all individuals stratified by subtype, with the poorly fitting subjects (those that had <0.5 probability of falling into any subtype) shown separately. All but one poorly fit subject exhibited very low SuStaIn stages. e, Probability of maximum likelihood subtype is low at early SuStaIn stage and quickly increases with increasing SuStaIn stage. f, Distribution of clinical diagnoses across SuStaIn stages. g, Distribution of clinical diagnoses across subtypes (same colors as in f). h, Distribution of maximum-likelihood subtype probabilities for each clinical diagnosis. i, Distribution of PCA and lvPPA subjects from the UCSF sample into each subtype. For boxplots in c,e,h, center line=median, box=inner quartiles, whiskers=extent of data distribution except *=outliers.
Extended Data Fig. 3 Regional comparisons.
Regional comparisons. Comparison of the mean tau-PET signal (tau-Z) across all ROIs, after adjustment for total cortical tau. A value of 0 represents regional tau Z-score proportionate to the average cortical tau Z-score in that subtype. The left panel represents left hemisphere, the right panel represents right hemisphere. Values represent means +/− SEM.
Extended Data Fig. 4 Subtypes observable across all contributing cohorts.
Subtypes observable across all contributing cohorts. The top panel shows the proportions of each subtype (plus S0) within each of the cohorts. All cohorts included individuals from each subtype. The bottom shows the mean tau Z image of each subtypes in a given cohort. Variation be observed across cohorts, particularly regarding phenotypic severity, but subtype patterns are fairly consistent.
Extended Data Fig. 5 Individual fit to stereotypical subtype progression.
Individual fit to stereotypical subtype progression. a) Progression plots are created for each subtyped individual based on their progression through events specific to their subtype. The outer images show regional tau z scores (see Extended Data Fig. 1) for an S2 (left) and S3 (right) individual. This data is summarized in lobar ROI z-scores (inner images). In progression plots under the images, each box represents a biomarker event, SuStaIn stage. A SuStaIn stage represents tau reaching a given severity (Z) score at a given region (see Extended Data Fig. 1). Filled (boxes indicate an individual fulfills the criteria for that SuStaIn stage. An empty (black) box indicates an individual does not. Note that each subtype has a different event order. b) A stepwise progression plot is shown for each subtype. Each row represents an individual, and each column represents SuStaIn stage. A perfect fit would be represented by an individual (row) having every box filled before a given stage, and no boxes filled after. y-axes (subjects) are sorted from the least (top) to most (bottom) stages fulfilled. Across the population, this should be represented as a stepwise progression. Each subtype demonstrates a stepwise progression indicating good general fit. The average subject fit imperfection was 2.1 boxes.
Extended Data Fig. 6 Replication using different initial parameters.
Replication using different initial parameters. SuStaIn creates nearly identical subtypes when initialized with different parameters (Supplementary Table 5) Methods: Replication Analysis). SuStaIn was rerun allowing a data-driven methodology to determine the number and value of z-score waypoints for each ROI. a) Qualitative contrasts of each subtype as defined using the original (Orig) parameters and the new data-driven (DD) parameters, where maps show regions significantly different between one subtype and all others (excluding S0) within the cohort (after FDR correction). b) Confusion matrix comparing subtypes identified in the original (orig) sample (y-axis), and subtypes separately identified in the data-driven parameter replication sample (x-axis). Values represent spatial correlation between average regional tau for each subtype. Values along the diagonal indicates similarity between the same subtype across both parameter sets.
Extended Data Fig. 7 Stability of subtypes across train-test split and replication datasets.
Stability of subtypes across train-test split and replication datasets. (Top) Cortical renders showing, for each subtype across each dataset, regions with significantly different tau-PET signal compared to other within-dataset subtypes after FDR correction. Hot regions show greater tau-PET signal, whereas cooler regions show lower signal. Remarkable similarity can be observed across subtypes, except S4, where lateralization switches from left to right. (Bottom) A heatmap showing similarity (spatial correlation) between subtypes across all four datasets. The diagonal represents identity, whereas outlined boxes represent comparisons of the same subtype across datasets.
Extended Data Fig. 8 Subtypes present with differing clinical profiles.
Subtypes present with differing clinical profiles. For all plots, a * below a box indicates the subtype is significantly different (corrected p < 0.05) from other subtypes combined (one vs. all), while a χ represents a trend (p < 0.1). Thick horizontal lines above boxes indicate significant (p < 0.05) differences between two subtypes (one vs one). Dashed horizontal lines represent the mean of the S0 group (controlling for covariates), where relevant. All statistics are adjusted for demographics, disease status, cohort and SuStaIn stage. For boxplots, the center line=median, box=inner quartiles, whiskers=extent of data distribution except *=outliers.
Extended Data Fig. 9 Lateralization across disease progression as measured with SuStaIn stage.
Lateralization across disease progression as measured with SuStaIn stage. a, Tau lateralization was measured as the mean left to right ratio of scores for all ten tau features. Higher positive numbers represent greater left hemisphere tau lateralization, whereas lower negative numbers represent greater right hemisphere lateralization. The progression of laterality over SuStaIn stage was visualized for each subtype. Lateralization generally increased with increasing SuStaIn stage. In some subtypes (particularly S2 and S3), strong lateralization was seen in both hemispheres later stages. b, The absolute (that is agnostic to hemisphere) lateralization was visualized against SuStaIn stage, indicating general increase in lateralization with more severe tau expression. c, A three-way relationship between age, SuStaIn stage and absolute lateralization is visualized, indicating these relationships covary but are independent of one another. For b, confidence interval represents 95% around line-of-best-fit across 1000 bootstrap samples.
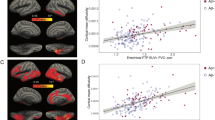
Extended Data Fig. 10 Replication of subtype-specific epidemic spreading model.
Replication of subtype-specific epidemic spreading model. We repeated analyses from Fig. 4, this time using functional connectivity from a sample of elderly healthy and MCI individuals, over a higher-resolution cortical atlas, as the connectome input to the model. The ESM was fit separately for each subtype; once using an entorhinal cortex epicenter (a), gray], and once with a subtype-specific best-fitting epicenter (b), blue]. For each plot, each dot represents a region. The x-axis represents the mean simulated tau-positive probabilities across the population, while the y-axis represents mean observed tau-positive probability. Each column represents a subtype. Confidence interval represents 95% CI around line-of-best-fit across 1000 bootstrap samples c) Visualization of the best-fitting epicenter selected by the model. d) For each subtype, the probability that each region’s best fitting epicenter for that subtype, based on bootstrap resampling (1000 samples).
Supplementary information
Supplementary Information
Supplementary Notes 1–3 and Tables 1–6.
Rights and permissions
About this article
Cite this article
Vogel, J.W., Young, A.L., Oxtoby, N.P. et al. Four distinct trajectories of tau deposition identified in Alzheimer’s disease. Nat Med 27, 871–881 (2021). https://doi.org/10.1038/s41591-021-01309-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41591-021-01309-6
This article is cited by
-
Text mining and portal development for gene-specific publications on Alzheimer’s disease and other neurodegenerative diseases
BMC Medical Informatics and Decision Making (2024)
-
Epilepsy and epileptiform activity in late-onset Alzheimer disease: clinical and pathophysiological advances, gaps and conundrums
Nature Reviews Neurology (2024)
-
Data-driven modelling of neurodegenerative disease progression: thinking outside the black box
Nature Reviews Neuroscience (2024)
-
Multi-modal Neuroimaging Phenotyping of Mnemonic Anosognosia in the Aging Brain
Communications Medicine (2024)
-
Longitudinal inference of multiscale markers in psychosis: from hippocampal centrality to functional outcome
Molecular Psychiatry (2024)