Rat brain injuries 'plugged' with lab-grown human minibrains in world-first experiment
Scientists transplanted human brain organoids into rats to repair injuries to their visual processing systems.
Miniature, lab-grown models of the human brain's wrinkled surface can be used to patch injuries in the brains of living rats and thus repair broken connections in the rodents' sensory processing systems, a new study shows. Someday, such minibrains — known as brain organoids — could potentially be used to mend the brains of human patients, too, the study authors propose.
"I see this as the first step in developing a new strategy for repairing the brain," said Dr. Han-Chiao Isaac Chen, the study's senior author and an assistant professor of neurosurgery at the University of Pennsylvania Perelman School of Medicine.
Eventually, organoids could be used to restore the brain's function following a traumatic injury, invasive surgery or stroke, or to help combat the effects of neurodegenerative diseases, such as Parkinson's, Chen told Live Science. However, we're many years away from applying the technology in humans, he said.
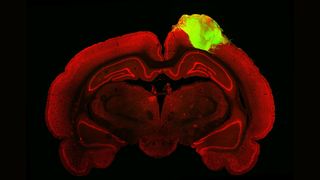
In their new study, published Thursday (Feb. 2) in the journal Cell Stem Cell, Chen and his colleagues demonstrated that brain organoids grown from human stem cells can be transplanted into an injured rat's visual cortex, where information from the eyes first gets sent for processing.
Related: Lab-grown mini 'brains' of humans and apes reveal why one got so much bigger
When light hits the retina in the eye, an electrical message zips to the "primary" visual cortex, which begins parsing the basic features of whatever's in front of the eye. Those data then get forwarded to the "secondary" visual cortex, which takes the analysis a step further. In the new study, adult rats sustained a major injury to the secondary visual cortex, and researchers essentially used an organoid to plug the resulting hole in the brain.
In prior research, scientists have transplanted individual brain cells into healthy rodents of varying ages and organoids into the brains of very young, uninjured rodents; by transplanting organoids into older, injured rats, this study signals another step toward using organoids to repair brain injuries, Chen said.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
The team grew their organoids from a type of human stem cell that can give rise to many different kinds of cells. For 80 days, the researchers had used chemical cues to coax these stem cells into 3D clumps that contained many, but not all, of the cell types found in the human cerebral cortex, the brain's wrinkled outer layer. The cortex contains six distinct layers of tissue, and by day 80, the lab-grown organoids bore similar, but somewhat rudimentary, layers.
"This structure is really very important for defining how the brain actually functions," Chen said of the organoids' 3D architecture. However, although the clumps of tissue resemble a real cortex in many respects, "they're not perfect, by any means," he added.
To transplant each organoid into a rat brain, the team removed a piece of each rodent's skull, placed the organoid inside and sealed the hole with a protective cap. The rats received immune-suppressing drugs during and after the procedure, to prevent their bodies from rejecting the transplant.
Over the following three months, the rats' blood vessels infiltrated the organoids, and in turn, the organoids' cells became physically intertwined with the rest of the rodents' visual processing systems.
The organoids grew slightly larger during this time, gaining new cells and extending wires to link to the rats' brain cells. The researchers mapped out these new connections using a fluorescent tracer, which revealed that the organoids had successfully connected to the retina through this network of wires. What's more, the researchers showed the rats visual stimuli — including flashing lights and black and white bars on a screen — and found that their organoids activated in response, as an intact visual cortex would be expected to.
The team didn't run vision or behavioral tests on the rats to investigate how their ability to see changed following their injuries or their transplant procedures. The researchers are now working on such assessments. In the future, they plan to test whether organoids can be similarly integrated into other parts of the brain, such as the motor cortex, which controls movement, and to study what factors control the speed and extent of that integration.
In addition, the team hopes to improve upon brain organoids such that they better mimic a real human brain. "We want a substrate that more faithfully replicates what the brain looks like," as in theory, that should make the organoids more useful for future brain repairs, Chen said.

Nicoletta Lanese is the health channel editor at Live Science and was previously a news editor and staff writer at the site. She holds a graduate certificate in science communication from UC Santa Cruz and degrees in neuroscience and dance from the University of Florida. Her work has appeared in The Scientist, Science News, the Mercury News, Mongabay and Stanford Medicine Magazine, among other outlets. Based in NYC, she also remains heavily involved in dance and performs in local choreographers' work.
